1-833-ZEPOSIA
ZEPOSIA is a once-daily pill for adults with moderate to severe ulcerative colitis (UC).
Take as directed by your doctor if certain liver problems exist.
ZEPOSIA is a once-daily pill for adults with moderate to severe ulcerative colitis (UC).
Take as directed by your doctor if certain liver problems exist.
The first treatment of its kind for UC
ZEPOSIA is the first S1P receptor modulator approved for UC. It targets a specific part of immune cells called S1P receptors, which play a role in the UC inflammation process.
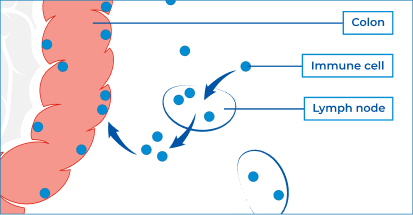
The immune system is the body’s natural defense against infection.
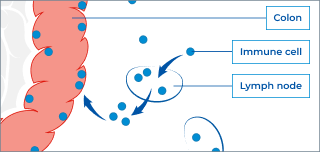
Immune cells circulate in the bloodstream, some of them passing through small glands called lymph nodes, traveling throughout the body to wherever they are needed.
If a problem is detected, like an infection, immune cells circulating in the body recruit more cells from the lymph nodes to help fight it off.
The exact cause of UC is unknown, but it is believed to be related to an irregular immune response. In UC, the immune system responds incorrectly and recruits immune cells to the colon (large intestine and rectum).
This results in ongoing (chronic) inflammation that damages the colon and causes the symptoms that people with UC may experience.
Learn more about UC
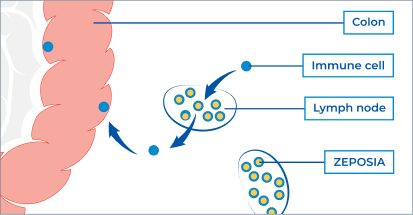
*The exact way ZEPOSIA works is not known. However, by binding to S1P receptors on immune cells, ZEPOSIA is thought to act as a gatekeeper, helping to keep these cells from moving out of the lymph nodes and into the colon.
By keeping these cells out of the intestines, ZEPOSIA may help prevent them from causing the damaging inflammation seen in UC.