Important facts about
ZEPOSIA® (ozanimod)
This is a summary of important information that you need to know about ZEPOSIA. Your healthcare provider can work with you to help answer any questions you may have about this medication. Keep this information in a safe place, so you can refer to it before and during your treatment.
Look out for the following icons as you
read:

Talk to your healthcare provider

Call a healthcare provider right away

Helpful information to remember
What is ZEPOSIA?
ZEPOSIA® (ozanimod) is a prescription medicine used to treat:
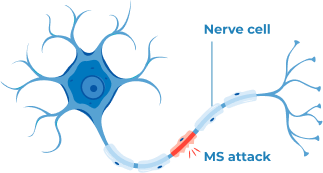
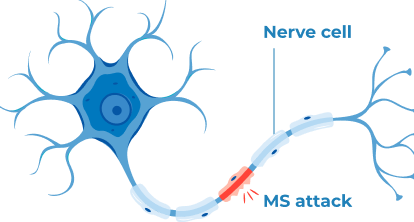
Adults with relapsing forms of multiple sclerosis (MS), including:
- Clinically Isolated Syndrome (CIS),
- Relapsing-Remitting MS Disease (RRMS), and
- Active Secondary Progressive MS Disease (SPMS)
Adults with moderately to severely active ulcerative colitis (UC)
It is not known if ZEPOSIA is safe and effective in children under 18 years of age.
- ZEPOSIA should not be taken if:
- You have or have had problems with your heart or blood flow such as:
- A heart attack, chest pain (unstable angina), a stroke or mini-stroke (transient ischemic attack [TIA]), or certain types of heart failure in the last six months
- A history of certain types of irregular or abnormal heartbeat (arrhythmia) that is not corrected by a pacemaker
- You have untreated, severe breathing problems during your sleep (sleep apnea)
- You take certain medicines called monoamine oxidase (MAO) inhibitors (such as selegiline, phenelzine, linezolid)
- Talk to your healthcare provider before taking ZEPOSIA if you have any of these conditions, or don’t know if you have any of these conditions.
What is the most important information I should know about ZEPOSIA?
ZEPOSIA may cause serious side effects. A serious side effect is a side effect that can sometimes become life threatening and can lead to hospitalization or death. The serious side effects of ZEPOSIA may include:
Infections. ZEPOSIA can increase your risk of serious infections that can be life-threatening and cause death. ZEPOSIA lowers the number of white blood cells (lymphocytes) in your blood. Having fewer white blood cells weakens your immune system, and increases your risk of serious infections. Before starting ZEPOSIA, your healthcare provider may do a blood test to make sure that your white blood cells are not too low. After stopping ZEPOSIA, the number of white blood cells that you have in your blood usually goes back to normal within three months.
- Call your healthcare provider right away if you have any of the following symptoms of an infection during treatment with ZEPOSIA, and for three months after your last dose of ZEPOSIA:
- Fever
- Feeling very tired
- Flu-like symptoms
- Cough
- Painful and frequent urination (signs of a urinary tract infection)
- Rash
- Headache with fever, neck stiffness, sensitivity to light, nausea, or confusion (these may be symptoms of meningitis, an infection of the lining around your brain and spine)
Your healthcare provider may delay starting, or may stop your ZEPOSIA treatment if you have an infection.
Progressive multifocal leukoencephalopathy (PML). PML is a rare brain infection that usually leads to death or severe disability. ZEPOSIA can increase your risk for PML. PML usually happens in people with weakened immune systems but has happened in people who do not have weakened immune systems.
- Call your healthcare provider right away if you have any new or worsening symptoms of PML that have lasted several days. Symptoms get worse over days to weeks. These symptoms include:
- Weakness on one side of your body
- Loss of coordination in your arms or legs
- Decreased strength
- Balance problems
- Changes in your vision
- Changes in thinking or memory
- Confusion
- Changes in your personality
Your healthcare provider will stop treatment with ZEPOSIA if you are showing symptoms of PML.
Slow heart rate (also known as bradyarrhythmia) when you start taking ZEPOSIA. ZEPOSIA may cause your heart rate to slow down temporarily, especially during the first eight days that you start taking it. Before starting ZEPOSIA, your healthcare provider will do a test called an electrocardiogram (ECG) to measure the electrical activity of your heart.
- Call your healthcare provider if you have any of these symptoms:
- Feeling dizzy
- Feeling lightheaded
- Feeling tired
- Feeling like your heart is beating slowly or skipping beats
- Shortness of breath
- Feeling confused
- Chest pain
Your healthcare provider will increase your dosage slowly to reduce the risk of slow heart rate. It is important that you follow directions from your healthcare provider when starting ZEPOSIA and if you miss a dose. Please see additional information on taking ZEPOSIA below.
Liver problems. ZEPOSIA may cause liver damage. Your healthcare provider will do blood tests to check your liver’s health before you start taking ZEPOSIA and periodically during treatment.
- Call your healthcare provider right away if you have any of these symptoms of liver problems:
- Unexplained nausea
- Vomiting
- Dark colored urine
- Pain in the stomach (abdominal) area
- Feeling tired
- Loss of appetite
- Yellowing of the whites of your eyes or skin
Increased blood pressure. ZEPOSIA can cause your blood pressure to go up. Your healthcare provider should check your blood pressure while you take ZEPOSIA.
Breathing problems. Some people who take ZEPOSIA feel as though they cannot catch their breath (shortness of breath).
- Call your healthcare provider right away if you have new or worsening breathing problems.
A problem with your vision called macular edema. ZEPOSIA may cause swelling in the back of the eye (macula). Macular edema can cause some of the same vision symptoms as an MS attack (optic neuritis). You may not notice any symptoms with macular edema. Your healthcare provider should test your vision around the time you start taking ZEPOSIA, periodically while you continue taking ZEPOSIA, and at any time you notice vision changes during treatment with ZEPOSIA. Your chance of developing macular edema is higher if you have diabetes or have had uveitis (a type of inflammation of your eye).
- Call your healthcare provider right away if you have any of these symptoms:
- A blind spot, blurriness, or shadows in the
center of your vision
- Sensitivity to light
- Unusually colored vision
Types of skin cancer, including basal cell carcinoma, melanoma, and squamous cell carcinoma. Tell your healthcare provider if you have any changes in your skin, including changes in a mole, a new darkened area on your skin, a sore that does not heal, or growths on your skin, such as a bump that may be shiny, pearly white, skin-colored, or pink. Your doctor should check your skin for any changes at the start of and during treatment with ZEPOSIA. Limit the amount of time you spend in sunlight and ultraviolet (UV) light. Wear protective clothing and use a sunscreen with a high sun protection factor.
Swelling and narrowing of blood vessels in your brain. A condition called Posterior Reversible Encephalopathy Syndrome (PRES) is a rare condition of ZEPOSIA and other drugs like it. If left untreated, it may lead to a stroke. The symptoms of PRES usually get better once you stop taking ZEPOSIA.
- Call your healthcare provider right away if you have any of these symptoms:
- Sudden severe headache
- Sudden confusion
- Sudden changes or loss of vision
- Seizure
Your healthcare provider will test to see if you have any symptoms of PRES.
If you take or have previously taken ZEPOSIA for multiple sclerosis (MS): You may have severe worsening of MS symptoms after stopping ZEPOSIA. Your symptoms of MS may return and become worse compared to before or during treatment.
- Talk to your healthcare provider before you stop taking ZEPOSIA for any reason. Tell your healthcare provider if you have worsening symptoms of MS after stopping ZEPOSIA.
What are the most common side effects of ZEPOSIA?
The most common side effects of ZEPOSIA can include:
- Colds or infections that affect the nose, throat, and sinuses (upper respiratory tract infection)
- Elevated liver enzymes
- Sudden drops in blood pressure when you stand up (orthostatic hypotension), which can feel like dizziness or lightheadedness
- Painful and frequent urination (signs of urinary tract infection)
- Back pain
- High blood pressure
- Headache
These are not all of the possible side effects of ZEPOSIA.
- Talk to your healthcare provider for more information or advice about side effects. You are encouraged to report side effects of prescription drugs to the FDA by visiting www.fda.gov/medwatch or calling 1-800-FDA-1088.
What should I discuss with my healthcare provider before receiving ZEPOSIA?
- Talk to your healthcare provider about all of your medical conditions, including if you have:
- A recent fever or infection
- A disease that makes you unable to fight infections
- Problems with your heart, which may include:
- A slow heart rate
- An irregular or abnormal heartbeat (arrhythmia)
- Heart attack, or chest pain
- High blood pressure
- A history of stroke
- Liver problems
- Breathing problems, while awake or sleeping
- Eye problems, especially eye inflammation (called uveitis)
- Skin cancer (currently or in the past), including basal cell carcinoma (BCC), melanoma, or squamous cell carcinoma (SCC)
- Diabetes
- Talk to your healthcare provider if you have had chickenpox, or have received the vaccine for chickenpox.
Your healthcare provider may do a blood test for the chickenpox virus. You may need to get the full course of the chickenpox (Varicella Zoster Virus) vaccine, and then wait one month before you start taking ZEPOSIA.
- Talk to your healthcare provider about all the medicines you are taking or have recently taken, including:
- Prescription medicines
- Over-the-counter medicines
- Vitamins
- Herbal supplements
It is especially important to tell your healthcare provider if you take, or have taken any medicines that:
- Affect or lower your immune system (such as alemtuzumab)
- Control your heart rhythm (such as antiarrhythmics) or heartbeat
- Promote or inhibit CYP2C8 activity (such as rifampin or gemfibrozil)
- Are opioids
- Treat depression
- Treat Parkinson’s disease
- Control your heart rate and blood pressure (such as beta blocker and calcium channel blocker medicines)
- Are medicines called monoamine oxidase (MAO) inhibitors (such as selegiline, phenelzine, or linezolid)
- Talk to your healthcare provider if you are not sure if you take any of these medications. Using ZEPOSIA with other medicines can cause serious side effects. Keep a list of the medicines you take to show your healthcare provider and pharmacist.
- Talk to your healthcare provider if you have received a vaccine in the past 30 days, or are scheduled to receive a vaccine (immunization). ZEPOSIA may cause vaccines to be less effective.
You should not receive live vaccines during treatment with ZEPOSIA, for at least one month before taking ZEPOSIA, and for three months after you stop taking ZEPOSIA. Live vaccines are vaccines that use a small amount of the weakened virus. Some common live vaccines (among others) include:
- Measles, mumps, and rubella (MMR)
- Intranasal flu vaccine
What should I discuss with my healthcare provider about pregnancy, birth control, and breastfeeding?
- Talk to your healthcare provider if:
- You are pregnant or plan to become pregnant — ZEPOSIA may harm your unborn baby.
If you are able to become pregnant, you should use effective birth control during your treatment with ZEPOSIA and for three months after you stop taking ZEPOSIA.
- Talk to your healthcare provider about birth control methods you can use with ZEPOSIA.
- You are breastfeeding or plan to breastfeed — It is not known if ZEPOSIA passes into your breast milk.
- Talk to your healthcare provider about the best way to feed your baby if you take ZEPOSIA.
- Call your healthcare provider right away if you become pregnant or think you are pregnant while taking ZEPOSIA, or within three months after you stop taking it.
If you are taking ZEPOSIA for multiple sclerosis: Talk to your healthcare provider about registering for the ZEPOSIA Pregnancy registry. This registry is for people with multiple sclerosis who become pregnant during treatment with ZEPOSIA. Its purpose is to collect information about you and your baby’s health. Either you or your healthcare provider can enroll you in this registry by calling 1-877-301-9314 or visiting www.zeposiapregnancyregistry.com.
How will I take ZEPOSIA?
Take ZEPOSIA exactly as your healthcare provider tells you. Your healthcare provider may change your dose schedule (frequency) if certain liver problems exist.
ZEPOSIA is an opaque capsule filled with a white to off-white powder. It comes in three dosage strengths (0.23 mg, 0.46 mg, and 0.92 mg) that are different colors. The capsules all have “OZA” and their dosage strength in mg printed in black ink.
Inactive ingredients: colloidal silicon dioxide, croscarmellose sodium, magnesium stearate, and microcrystalline cellulose
Capsule shell inactive ingredients: black iron oxide, gelatin, red iron oxide, titanium oxide, and yellow iron oxide
- Do swallow ZEPOSIA capsules whole
- Do take ZEPOSIA with or without food
- Do take ZEPOSIA exactly as your healthcare provider tells you
- Do not skip a dose of ZEPOSIA
- Do not stop taking ZEPOSIA without talking with your healthcare provider first
Starting ZEPOSIA (days 1 to 7): Your treatment with ZEPOSIA begins with a 7-day Starter Pack. This pack includes all of the pills that you need for the first 7 days of treatment, and helps to gradually increase your dosage of ZEPOSIA. Be sure to follow the instructions written on the pack and take the pills in the correct order.
One 0.23 mg capsule one time per day
This capsule is light grey
One 0.46 mg capsule one time per day
This capsule is half-light grey and half-orange
Continuing ZEPOSIA (days 8 onwards): After finishing your first week of treatment, you will take your regular dose of ZEPOSIA.
One 0.92 mg capsule one time per day, or as directed by your healthcare provider
This capsule is orange
What if I miss a dose of ZEPOSIA?
Do not take an extra dose.
During days 1– 14 (first two weeks) of starting treatment: If you miss one or more doses, let your healthcare provider know. You will need to restart your ZEPOSIA treatment and get a new 7-day Starter Pack.
After the first 14 days of treatment: If you miss one dose of ZEPOSIA, take one capsule at your next usual time. You can continue your treatment as planned.
How should I store ZEPOSIA?
ZEPOSIA capsules should be stored at room temperature between 68°F to 77°F (20°C to 25°C).
Keep ZEPOSIA and all medicines out of reach of children.
ZEPOSIA® and the ZEPOSIA® logo are trademarks of Celgene Corporation, a Bristol Myers Squibb company. All other trademarks listed are the property of their respective owners.